Eczema is a chronic inflammatory skin condition characterized by areas of dry skin that are red and intensely itchy.
The affected skin may ooze, become scaly, crusted, or hardened. Symptoms can range from mild to severe and the condition can negatively impact quality of life. Eczema can occur anywhere on the skin and is commonly found on the flexors (bends of the arms and backs of the knees).
There are many types of eczema, with the most common one being atopic dermatitis (AD). Atopy refers to a hereditary tendency toward eczema, asthma, and allergic rhinitis (hay fever). People with eczema may suffer with one of the other atopic diseases.
Atopic dermatitis, the most common form of eczema, is estimated to affect 15% of children and 4% of adults in Canada, with the majority of cases being mild to moderate in severity (Gooderham et al., 2025).¹
There are genetic, immunological, and environmental factors that play a role in eczema.
Eczema can come and go and can migrate around the body—just as one area of affected skin clears up, another may develop. This is the chronic nature of the disease. When the skin cycles back to inflammation, the patient is experiencing a flare-up. Contrary to popular belief, foods or food allergies do not cause eczema, even though a certain food may contribute to an acute flare of eczema.
Flare-ups can be prompted by environmental elements or “triggers” such as certain soaps, clothing fabrics, deodorants, carpet fibres, dust, and others.
Sometimes a flare-up will occur, however, with no discernible trigger. Overheating, excessive sweating, low humidity, certain foods, infection, and stress can also contribute to flare-ups. When the skin becomes irritated by any one of these irritants, it itches, causing the sufferer to scratch the affected area. Scratching makes the condition worse and the skin becomes inflamed and reddened, aggravating the itch. This is called the “itch-scratch cycle” and can become severe and cause pain.
Look around you and write down all the possible things in your surroundings that could be contributing to your flare-ups. For example, do you experience a flare-up or worsening of your eczema when you wear a certain sweater? Is your eczema worse in the winter? Do you itch on the days when you clean your house? Does perfume irritate your skin?
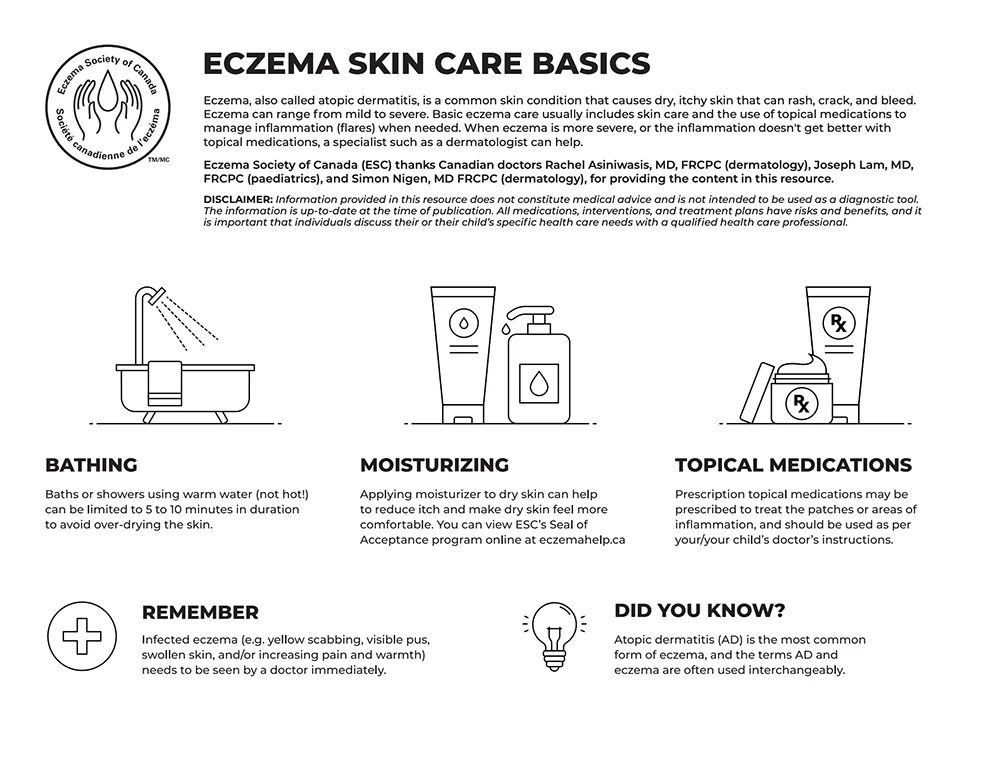
Controlling factors in your environment can help minimize flare-ups. By minimizing or eliminating your triggers, you can help to reduce the number of flare-ups experienced. One of the frustrating parts of eczema is that flare-ups can still occur even when you are diligently avoiding triggers and taking care of your skin. Keeping your skin moist is your first line of defense against eczema.
Certain foods can trigger a flare-up, just like other environmental triggers. This can occur by eating the trigger food, or by skin contact with the food during preparation or during eating (on the hands and around the mouth). It is important to note that food allergies do not cause eczema, however, foods can trigger a flare-up. It is not recommended to undertake food elimination diets or to withhold specific foods or entire food groups for long periods of time without consulting your doctor or your allergist to confirm that there is in fact an allergy to that food.
Atopic eczema is a chronic, recurring condition with “flares” (active or new areas of eczema-affected skin) that look red, scaly, and/or bumpy, and remissions (when eczema is not as active). Some people always seem to have some active areas.
There are no definite cures for eczema although patients can achieve excellent control and live quite comfortably.
When one member of the family suffers with eczema, the whole family suffers. Rigorous moisturizing and skin care treatment regimens, constant monitoring of the condition, lifestyle changes to avoid triggers, and sleepless nights can greatly impact the quality of life for all members of the family.
Some complications of eczema include skin infections, eczema herpeticum, fluid-filled dermatitis, and eye complications.
Scratching that is associated with eczema can break the skin causing open sores which can then become infected. This can cause mild or more serious infections. See a physician if there is swelling, pain, crusting, or oozing of the eczema.

Skin that becomes infected with the herpes simplex virus (the virus that causes cold sores) is called eczema herpeticum. The symptoms may include painful pus or fluid-filled blisters or sores, which may be accompanied by fever, tiredness, and swollen glands. Prompt treatment is very important, as the infection can spread to the eyes or internal organs, causing serious problems.
Caution should be taken around anyone with a cold sore; kissing and skin-to-skin contact should be avoided. Take extra caution with infants and children, especially those with eczema and/or open areas on their skin. Sometimes, with infants and small children, contact with the herpes simplex virus can be fatal. See a doctor immediately if there are concerns.

Long-term itching and scratching of the skin can lead to an increased sensation of itch, which could possibly lead to neurodermatitis (also known as lichen simplex chronicus). The areas of skin that are frequently scratched become thick and leathery in appearance and can be red and darker than the rest of the skin. Persistent scratching can lead to permanent changes in skin colour. See a physician if experiencing intense itch and/or there are noticeable changes in the skin.

In rare cases, severe atopic dermatitis can lead to eye complications, which could potentially cause permanent eye damage. See a physician if you are experiencing eye watering, inflammation around the eye, and eye discharge.
Learn about bathing, moisturizing, and eczema management, as well as common triggers and techniques to cope with itch.
Receive the latest on eczema management, free events, research and community news.