Frequent moisturization of the skin can be necessary in patients with eczema.
The natural skin barrier, which would normally trap moisture in the skin, doesn’t work well for patients with eczema. This leaves the skin dry, rough, and sensitive to irritants. It is a common myth that drinking an adequate amount of water during the day will hydrate the skin; however, applying a moisturizer frequently does help hydrate the skin.
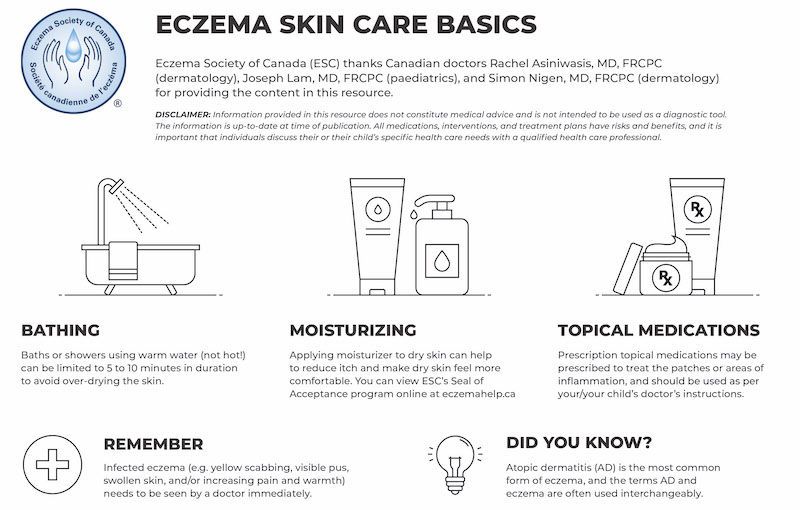
After bathing, gently pat the skin dry. Then follow your doctor’s recommendations for moisturizing and medication use (e.g., immediately applying your prescription treatments to the skin affected by eczema, and applying a moisturizer to areas of the skin that don’t have active eczema).
Daily baths or showers are reasonable for people with eczema; however, the duration of the bath or shower should be brief (5 to 10 minutes), and the bath or shower should be done with fresh, warm (not hot) water without additives such as soap or bubble bath.
It is important to understand that eczema is a chronic condition for which there is no cure. Therefore, it is equally important to understand how to manage the condition.
The goal of eczema management is to reduce the inflammation during acute flares. During periods of clear skin, the goal is to maintain that skin through moisturizer use.
Some eczema triggers may be avoidable (e.g., harsh soaps), but some triggers may be unavoidable (e.g., sweating for an athlete). Sometimes an eczema flare can occur with what seems like no trigger.
You can discuss your eczema and suitable medications with your or your child’s physician.
Medical treatment is an important part of controlling the inflammation of atopic dermatitis (AD) and should be used as prescribed by your health care provider to maximize benefits while minimizing potential side effects. Medical treatment of AD typically begins with topical medications that are applied to the skin. The good news is that there are many treatments for AD, including treatments for when AD is not getting better.
It is very important to share your treatment goals, what symptoms bother you, and what you would like to improve with your health care provider. It is also important to be honest about how you are using your treatment and how often you are using them (or if at all), as this can help your health care provider make the best recommendations for you or your child’s treatment plan.
Health Canada has approved many treatments for atopic dermatitis. Indication, including age and dose, will vary by treatment. Patients and caregivers can work with their health care provider to optimize their treatment plan. With all medications, there are benefits, risks, and side effects that should be discussed with your health care provider regarding your specific medication and condition.
Disclaimer: Information provided on this website does not constitute medical and is not intended to be used as a diagnostic tool. The information is up-to-date at time of publication. All medications, interventions, and treatment plans have risks and benefits, and it is important that individuals discuss their or their child’s specific health care needs with a qualified health care professional.
Topical corticosteroids (TCS) are common medications prescribed to treat AD and help to quickly reduce inflammation and itching. These medicines have been used to treat various skin conditions for many decades. The strengths of TCS range from mild to very potent and can be prepared as creams, ointments, foams, lotions, or shampoos, depending on the area of the body being treated. The more potent TCS medications should be used with caution and for short periods of time, and as with all medications, they should be used as per the prescriber’s instructions.
Topical calcineurin inhibitors (TCI) (e.g., Elidel® (pimecrolimus) and Protopic® (tacrolimus)) are non-steroid treatments for inflammation and itching associated with AD. They can be used for short, intermittent periods to manage flares and are sometimes used to prolong the time between flares (this is referred to as maintenance therapy). These medications work by quieting down the immune system reaction in the skin, which causes inflammation. Elidel® is a cream product that comes in one strength. Protopic® is an ointment product that comes in two different strengths.
Topical phosphodiesterase-4 (PDE4) inhibitors (e.g., EucrisaTM (crisaborole), Zoryve® (roflumilast) are topical medications for treating mild to moderate AD. These medications are not steroids and work to block an enzyme called phosphodiesterase 4 (PDE4 for short) from allowing too much inflammation to occur in the skin. Cells in our immune system produce PDE4, which promotes the production of cytokines (the proteins that contribute to inflammation). There are two topical PDE4 treatments approved in Canada, and they have different features. EucrisaTM is in an ointment formula, and Zoryve® is in a cream formula. Zoryve® has also been approved for seborrheic dermatitis as a stronger formula and prepared in a foam vehicle instead of a cream.
Topical Janus kinase (JAK) inhibitor medication (e.g. Opzelura® (ruxolitinib) is a cream that is approved for the treatment of mild to moderate AD for patients who are not adequately controlled with topical prescription therapies or when those therapies are not advisable (e.g., topical corticosteroids, topical calcineurin inhibitors). Topical JAK inhibitors are not topical steroids; they are targeted to work to block the overactive immune system pathways that cause inflammation in AD skin.
Topical antibiotics are prescribed for secondary infection, which can worsen the AD. They may make it more difficult for the condition to respond to treatment until the bacterial infection has been cleared. Topical antibiotic creams and ointments may treat localized areas of infected or resistant AD.
Oral antibiotics are prescribed for more significant skin infections. There is often secondary infection on the skin affected by AD, even when there may be no other obvious signs of infection. Oral antibiotics are preferred over topical antibiotics when the infection is severe or extensive.
Recent treatment guidelines do not recommend topical antihistamine use in AD. Oral antihistamines, both first and second-generation, are sometimes used for AD. There is not enough evidence to recommend using oral antihistamines for the treatment of AD, and they don’t treat the root cause of AD flares. Use of antihistamines for young children, such as those under age 6, is not generally recommended. Therefore, their use should be only under the supervision of a qualified health care provider. Always consult your healthcare provider to determine the best approach for your specific case.
Many patients can often manage their atopic dermatitis (AD) through a moisturizing regimen and by using topical medications when needed during flares. However, some individuals with a more severe form of the condition don’t have an adequate response and may benefit from more aggressive therapies. If you are struggling to manage your AD, talk to your health care provider about your options, as there are systemic therapies and other treatments, like phototherapy, that can significantly improve AD.
Health Canada has approved many treatments for atopic dermatitis. Indication, including age and dose, will vary by treatment. Patients and caregivers can work with their health care provider to optimize their treatment plan. With all medications, there are benefits, risks, and side effects that should be discussed with your health care provider regarding your specific medication and condition.
Cyclosporine, methotrexate, azathioprine, and mycophenolate mofetil are systemic therapies commonly used off-label for severe eczema by dermatologists. It is important to note that all of these medications can cause side effects and require regular monitoring. They should be used with caution and after discussion of their risks and benefits with your physician.
Phototherapy, specifically broad and narrow-band UVB light, can be helpful for its local immunomodulatory effect. Specific phototherapy units are used to treat the hands and the body. Speak to your health care provider about the possibility of phototherapy as a treatment option.
Oral corticosteroids (e.g., prednisone) are rarely used to treat AD and are reserved for intermittent use in the most severe cases during an acute flare. There are long-term side effects with prolonged use, and because AD is a chronic condition, this is not a permanent solution for severe chronic AD. Use of this medication is best based on the discretion of your health care provider.
Biologic drugs for AD (e.g., Adtralza® (tralokinumab), Dupixent® (dupilumab), and Ebglyss™ (lebrikizumab) are for patients with moderate to severe AD that do not improve enough with topical medications. Biologic drugs for AD are taken by a needle under the skin (‘subcutaneous’). These medications work in a more targeted way to stop the process of inflammation that occurs with AD. Several biologic medications are approved in Canada, and they all may work somewhat differently. A dermatologist or qualified specialist will guide their patients on the right treatment.
Oral JAK inhibitors (e.g., Rinvoq® (upadacitinib) and Cibinqo® (abrocitinib) are a class of medication to treat moderate to severe AD that are not adequately controlled with a systemic treatment or when the use of those therapies is inadvisable. Oral JAK inhibitors are taken by mouth as a pill and work to treat AD by acting on multiple inflammatory pathways at the same time. It is these overactive inflammatory pathways that cause the inflammation of AD.
Learn about bathing, moisturizing, and eczema management, as well as common triggers and techniques to cope with itch.